To facilitate minimally invasive surgical procedures that involve surgical navigation, it is essential to undertake patient registration beforehand. This process serves as the core function of every surgical navigation system, aiming to enhance the accuracy of intraoperative navigation and ensure the safety of the patient. To achieve these objectives, various of techniques have been devised and implemented, allowing for increased precision and improved outcomes in surgical procedures.
Marker-based patient registration method
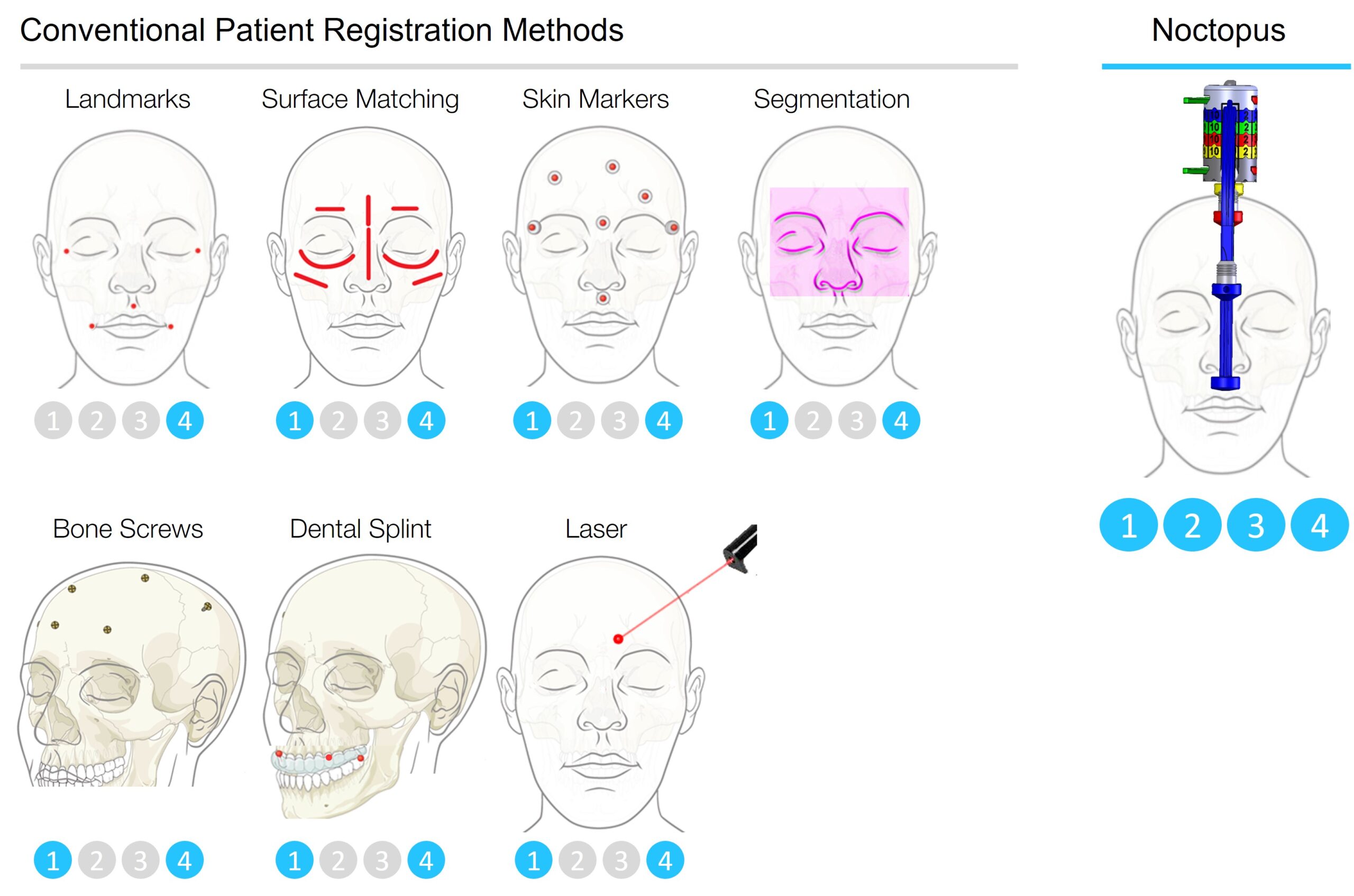
In marker-based registration, either anatomical landmarks, dental splints, skin adhesive markers, or invasive screw markers are used.
In the anatomical landmark method (also known as manual registration), suitable soft tissue and bone points are marked as registration points in the image data sets and then targeted intraoperatively on the patient using the tracked probe. Anatomical landmarks that are easy to identify and locate both in the image data and on the patient are considered particularly favorable. Additionally, these points should be in a fixed relationship to the anatomical structures in the head region. In this regard, the anterior nasal spine, the tip of the nose, the medial and lateral canthi, and the tragus tips are considered particularly suitable in the head area. The advantage of this method is the absence of the need for additional (invasive or non-invasive) markers and additional imaging with the markers. This procedure is hardly associated with additional burdens for the patient and the medical staff. However, the achievable accuracy is very limited because the registration points can only be selected at certain locations on the head. Therefore, the exact determination of the chosen registration markers in the image data sets is partially problematic, which consequently only allows for imprecise targeting of these virtually defined points on the patient’s head in some cases. The constantly varying patient anatomy presents the surgeon with new challenges in each registration process, requiring certain routines and exercises to achieve optimal navigation accuracy. Changes in patient anatomy after imaging, such as skin swelling or facial shifts, as well as a potentially prolonged duration of the registration process, also limit this type of registration. The literature on the average target accuracy of this procedure varies greatly from 0.9 mm to over 6 mm.
In the non-invasive dental splint method, registration markers are placed in a fixed and reproducible relationship to the patient’s head using a custom-fitted dental splint. To ensure this, a variety of different models have been designed. For example, a dental splint that could be fixed to the upper jaw of the patient using a vacuum. Other systems, such as the “Locking acrylic dental stent” (LADS), consist of multiple subunits for the front and back teeth that can be securely connected to each other, ensuring good stability. In contrast, there are models formed in one piece, such as the upper jaw thermoforming splint, as well as the upper jaw and vestibular silicone impression splint. The arrangement of the registration markers shows that a constellation of four alternately arranged markers has the highest navigation accuracy in the midface. Titanium screws are often used as registration markers because they can be clearly defined both in the image data and on the patient. The dental splint must be worn by the patient during imaging, can then be removed, and must be reinserted immediately before surgery. Assuming that the anatomy of the dentition does not change, a once-fitted dental splint can be reused if necessary. Studies have shown that dental splint registration is suitable for operations in the oral cavity, face, and orbit with an accuracy of 1 to 2 mm. However, with increasing distance from the registration markers, there is a significant decrease in precision in the area of the cranial vault, with deviations of 3 to 5 mm. The issue was addressed by using a frame construction attached to the dental splint, which, equipped with additional registration markers placed near the surgical area, allowed for more precise navigation in distant areas such as the temporal region. The optimal placement of the dental splint on the patient’s teeth during both imaging and intraoperative registration is crucial for the resulting precision. Even minimal deviations from the correct placement can greatly affect navigation accuracy. The dental status of the patient must also be taken into account with this method. Age-related or traumatic changes, poor dental stability, or the absence of teeth can restrict or even make the use of a dental splint impossible.
The skin adhesive marker method involves the distribution and application of special adhesive markers on the patient’s skin prior to image acquisition, which serve as registration markers. These markers must be easily identifiable both in the image data and on the patient’s body, and they should have a distinct structure, usually located in the center, that can be clearly identified as a registration point. In this regard, various marker systems have been developed, including radiopaque spheres, contrast-filled plastic tubes, and multipart products consisting of a base component attached to the skin and aluminum balls adapted to it. As with other marker-based registration procedures, the number and distribution of adhesive markers play a crucial role in the resulting navigation accuracy. The literature reports variations in marker accuracy ranging from 0.80 mm to 3.86 mm. Limitations of this method include the potential for skin displacement. Changes in skin turgor, wrinkles, and patient positioning can cause the adhesive markers to shift, making registration difficult or even impossible. There is also a risk of marker detachment between image acquisition and surgical intervention, although attempts have been made to enable reproducible marker positioning through visual markings.
The invasive screw marker method involves the placement of titanium screws in the patient’s skull bone, in varying numbers (at least 4), under local anesthesia prior to imaging. These screws serve as registration markers and remain in place until after the surgical procedure. Both in the image dataset and on the patient, these registration points must be clearly identified. Their unchanged position between imaging and surgery allows for a highly accurate correlation and precision between virtual and real patient anatomy. Changes in patient physiognomy, such as shifts in skin surface due to positioning, swelling (e.g., edema, hematomas, etc.), or facial injuries, do not affect the accurate capture of the registration markers. The average accuracy of this method is reported in the literature to be between 0.67 and 1.10 mm. Like any invasive procedure, the attachment of multiple screw markers carries the risk of wound infection, injury to anatomical structures such as nerves and blood vessels, and potential postoperative bleeding. Potential disadvantages of this method include skin irritations and residual scars.
Surface-based patient registration method
Surface-based methods involve surface detection through segmentation, laser-based, or pointer-based registration methods:
An alternative to marker-based methods are the surface-based registration methods. The basis for this concept of surface matching is a process known as segmentation. Using image data sets, 3D reconstructions, in this case of the patient’s head, particularly the face, can be generated by the computer. This virtual 3D model is then correlated with the captured facial contours of the real patient usually using the “Iterative Closest Point” (ICP) algorithm. All surface-based registration procedures have certain limitations. Changes in the surface structure of the patient’s face between data acquisition and surgical intervention (such as edema or changes in facial expression) have a significant impact on the resulting navigation accuracy. For this reason, any necessary intraoperative registration processes may be hardly possible if the patient’s anatomy deviates significantly from the previously captured image data due to the intervention, leading to errors that are twice as large as those using point pair matching with adhesive markers.
In the laser-based method, surface data is captured using a visible laser beam. Similar to a pointing instrument, the surgeon traces the facial contours of the patient in this semi-automatic procedure. It is important to capture distinct and individual structures of the patient’s anatomy that are uncovered by a thin layer of soft tissue and are hairless, as they accurately represent the profile. Examples of such regions include the bridge of the nose, the edges of the eye sockets, and the forehead. The reflected laser beams are detected by a camera system, and with the help of captured surface points, a virtual three-dimensional profile of the patient’s anatomy can be computed using computer assistance. The average accuracy of this method is reported in the literature to be between 1.0 – 2.8 mm, although there have been reports of deviations of up to 9 mm.
In the pointer instrument-based surface detection method, the distinctive facial contours of the patient are scanned with the tracked probe, and a varying number of surface points are registered. The same criteria for selecting the structures to be included apply as in laser-based surface detection. The accuracy of this method is reported in the literature to be between 1.81 and 4.90 mm. One difficulty in performing this procedure is the handling of the pointer instrument. During the registration process, it must neither exert excessive pressure on the soft tissues nor float in the air without contact with them.
Different patient registration methods listed above in the clinical practice aim to achieve increased accuracy in intraoperative 3D navigation and maximize patient safety. However, a high or submillimetric accuracy is only achieved when all four following criteria, which have been mathematically, methodically, and clinically proven, are simultaneously fulfilled:
1. The selected registration points should be able to be determined and localized as accurately as possible in both the virtual image data and on the patient.
2. The points should include as large a part of the surgical area as possible, distributed on a sphere-like surface around it and/or placed very close to it.
3. The distance between the center point of the registration points and the surgical area should be minimal as possible.
4. These points should not be collinearly arranged on the surgical area.
Conventional methods, due to technical, methodological and/or anatomical limitations, cannot fulfill all or only some of these requirements. Therefore, the achieved accuracies are very limited and only provide clinically satisfactory results in certain surgical areas.
Noctopus is the only system that resolves all the issues of the conventional registration techniques and fully satisfies all the known requirements for patient registration. By utilizing completely non-invasive Noctopus, surgical procedures can be performed with the utmost accuracy and confidentiality, ensuring the highest level of patient safety during surgical navigation.

